Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
2D vs 3D morphological analysis of dorsal root ganglia in health and painful neuropathy
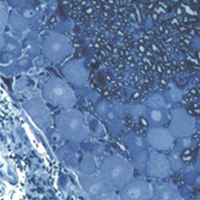
Dorsal root ganglia (DRGs) are clusters of sensory neurons that transmit the sensory information from the periphery to the central nervous system, and satellite glial cells (SGCs), their supporting trophic cells. Sensory neurons are pseudounipolar neurons with a heterogeneous neurochemistry reflecting their functional features. DRGs, not protected by the blood brain barrier, are vulnerable to stress and damage of different origin (i.e., toxic, mechanical, metabolic, genetic) that can involve sensory neurons, SGCs or, considering their intimate intercommunication, both cell populations. DRG damage, primary or secondary to nerve damage, produces a sensory peripheral neuropathy, characterized by neurophysiological abnormalities, numbness, paraesthesia and dysesthesia, tingling and burning sensations and neuropathic pain. DRG stress can be morphologically detected by light and electron microscope analysis with alterations in cell size (swelling/atrophy) and in different sub-cellular compartments (i.e., mitochondria, endoplasmic reticulum, and nucleus) of neurons and/or SGCs. In addition, neurochemical changes can be used to portray abnormalities of neurons and SGC. Conventional immunostaining, i.e., immunohistochemical detection of specific molecules in tissue slices can be employed to detect, localize and quantify particular markers of damage in neurons (i.e., nuclear expression ATF3) or SGCs (i.e., increased expression of GFAP), markers of apoptosis (i.e., caspases), markers of mitochondrial suffering and oxidative stress (i.e., 8-OHdG), markers of tissue inflammation (i.e., CD68 for macrophage infiltration), etc. However classical (2D) methods of immunostaining disrupt the overall organization of the DRG, thus resulting in the loss of some crucial information. Whole-mount (3D) methods have been recently developed to investigate DRG morphology and neurochemistry without tissue slicing, giving the opportunity to study the intimate relationship between SGCs and sensory neurons in health and disease. Here, we aim to compare classical (2D) vs whole-mount (3D) approaches to highlight “pros” and “cons” of the two methodologies when analysing neuropathy-induced alterations in DRGs.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.