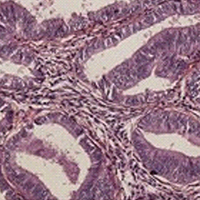
PD-L1 expression with QR1 and E1L3N antibodies according to histological ovarian cancer subtype: A series of 232 cases
Submitted: 1 October 2020
Accepted: 10 February 2021
Published: 10 March 2021
Accepted: 10 February 2021
Abstract Views: 949
PDF: 512
HTML: 14
HTML: 14
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- C. Dall'Oca, T. Maluta, F. Cavani, G.P. Morbioli, P. Bernardi, A. Sbarbati, D. Degl'Innocenti, B. Magnan, The biocompatibility of porous vs non-porous bone cements: a new methodological approach , European Journal of Histochemistry: Vol. 58 No. 2 (2014)
- J. Xue, H. Chen, L. Diao, X. Chen, D. Xia, Expression of Caveolin-1 in tongue squamous cell carcinoma by quantum dots , European Journal of Histochemistry: Vol. 54 No. 2 (2010)
- A.J.W. Pinto, I.F.G. de Amorim, L.J. Pinheiro, I.M.V.M. Madeira, C.C. Souza, H. Chiarini-Garcia, M.V. Caliari, W.L. Tafuri, Glycol methacrylate embedding for the histochemical study of the gastrointestinal tract of dogs naturally infected with Leishmania infantum , European Journal of Histochemistry: Vol. 59 No. 4 (2015)
- Letizia Ferroni, Chiara Gardin, Andrea De Pieri, Maria Sambataro, Elena Seganfreddo, Chiara Goretti, Elisabetta Iacopi, Barbara Zavan, Alberto Piaggesi, Treatment of diabetic foot ulcers with Therapeutic Magnetic Resonance (TMR®) improves the quality of granulation tissue , European Journal of Histochemistry: Vol. 61 No. 3 (2017)
- S.A. Ferreira, J.L.A. Vasconcelos, R.C.W.C. Silva, C.L.B. Cavalcanti, C.L. Bezerra, M.J.B.M. Rêgo, E.I.C. Beltrão, Expression patterns of α2,3-Sialyltransferase I and α2,6-Sialyltransferase I in human cutaneous epithelial lesions , European Journal of Histochemistry: Vol. 57 No. 1 (2013)
- R.J. BuÅ‚dak, M. Skonieczna, Å. BuÅ‚dak, N. Matysiak, Å. MielaÅ„czyk, G. Wyrobiec, M. Kukla, M. Michalski, K. Å»wirska-Korczala, Changes in subcellular localization of visfatin in human colorectal HCT-116 carcinoma cell line after cytochalasin B treatment , European Journal of Histochemistry: Vol. 58 No. 3 (2014)
- Yan Yan Li, Ya Ping Feng, Li Liu, Jin Ke, Xing Long, Inhibition of HMGB1 suppresses inflammation and catabolism in temporomandibular joint osteoarthritis via NF-κB signaling pathway , European Journal of Histochemistry: Vol. 66 No. 3 (2022)
- C. Severi, R. Sferra, A. Scirocco, A. Vetuschi, N. Pallotta, A. Pronio, R. Caronna, G. Di Rocco, E. Gaudio, E. Corazziari, P. Onori, Contribution of intestinal smooth muscle to Crohn's disease fibrogenesis , European Journal of Histochemistry: Vol. 58 No. 4 (2014)
- T. A. Osman, G. Øijordsbakken, D. E. Costea, A. C. Johannessen, Successful triple immunoenzymatic method employing primary antibodies from same species and same immunoglobulin subclass , European Journal of Histochemistry: Vol. 57 No. 3 (2013)
- T. Al-dhohorah, M. Mashrah, Z. Yao, J. Huang, Aberrant DKK3 expression in the oral leukoplakia and oral submucous fibrosis: a comparative immunohistochemical study , European Journal of Histochemistry: Vol. 60 No. 2 (2016)
<< < 3 4 5 6 7 8 9 10 11 12 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejh.2021.3185
https://doi.org/10.4081/ejh.2021.3185










