Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Efficacy of immunohistochemical staining in detecting Helicobacter pylori in Saudi patients with minimal and atypical infection
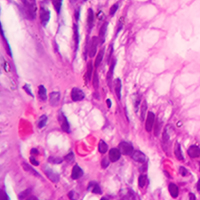
Gastric Helicobacter pylori infection is diagnosed based on histopathological evaluation of gastric mucosal biopsies, urease test, urea breath test, H. pylori culturing, or direct detection using polymerase chain reaction (PCR). This study aimed to evaluate the efficacy of immunohistochemical (IHC) staining in detecting H. pylori in gastric biopsies from patients with chronic gastritis and minimal or atypical infection. Gastric biopsies from 50 patients with chronic gastritis were subjected to routine haematoxylin and eosin (H-E), modified Giemsa, and IHC staining. The results of staining were compared with those of quantitative real-time PCR (qRT-PCR). The qRT-PCR analysis identified 32 (64%) H. pylori-positive cases, whereas IHC, H-E, and modified Giemsa staining identified 29 (58%), 27 (54%), and 21 (42%) positive cases. The sensitivity of IHC staining (87.50%) was higher than that of H-E (59.38%) and modified Giemsa (43.75%) staining. The specificity of H-E, modified Giemsa, and IHC staining was 55.56%, 61.11%, and 94.44%, respectively. IHC staining exhibited the highest diagnostic accuracy (90%), followed by H-E (58%) and modified Giemsa (50%) staining. Active gastritis, intestinal metaplasia, and lymphoid follicles were detected in 32 (64%), 4 (8%), and 22 (44%) cases, respectively, and all of these cases were H. pylori positive. In contrast to routine H-E and modified Giemsa staining, IHC allows for the accurate H. pylori detection in cases with minimal or atypical infection. Moreover, IHC can be an alternative diagnostic method to qRT-PCR for detection of H. pylori in such cases.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.