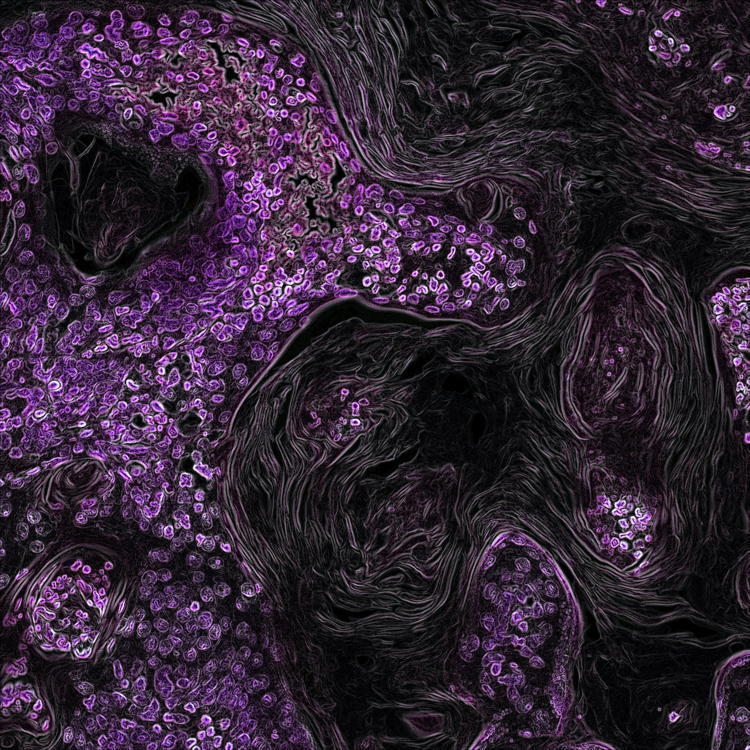
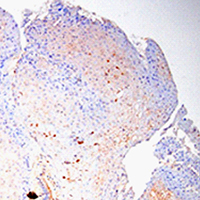
HPV infection upregulates the expression of ZNT-1 in condyloma acuminatum
Submitted: 14 February 2021
Accepted: 13 April 2021
Published: 28 April 2021
Accepted: 13 April 2021
Abstract Views: 974
PDF: 510
HTML: 10
HTML: 10
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- C Foglieni, S Scabini, D Belloni, F Broccolo, P Lusso, MS Malnati, E Ferrero, Productive infection of HUVEC by HHV-8 is associated with changes compatible with angiogenic transformation , European Journal of Histochemistry: Vol. 49 No. 3 (2005)
- A Icaro Cornaglia, M Casasco, F Riva, A Farina, L Fassina, L Visai, A Casasco, Stimulation of osteoblast growth by an electromagnetic field in a model , European Journal of Histochemistry: Vol. 50 No. 3 (2006)
- RM Ruggeri, S Sciacchitano, F Trimarchi, G Barresi, M Trovato, Expression of hepatocyte growth factor in Hashimoto’s thyroiditis with nodular lesions , European Journal of Histochemistry: Vol. 51 No. 3 (2007)
- CN Zanuzzi, PA Fontana, CG Barbeito, EL Portiansky, EJ Gimeno, Paneth cells: histochemical and morphometric study in control and Solanum glaucophyllum intoxicated rabbits , European Journal of Histochemistry: Vol. 52 No. 2 (2008)
- RG Steinbeck, Pathologic mitoses and pathology of mitosis in tumorigenesis , European Journal of Histochemistry: Vol. 45 No. 4 (2001)
- S Passinen, T Ylikomi, Evidence for the existence of an oligomeric, non-DNA-binding complex of the progesterone receptor in the cytoplasm , European Journal of Histochemistry: Vol. 47 No. 3 (2003)
- M Biggiogera, L Cocco, FA Manzoli, Structure and function of the cell nucleus , European Journal of Histochemistry: Vol. 48 No. 1 (2004)
- EV Sheval, MA Polzikov, MOJ Olson, OV Zatsepina, A higher concentration of an antigen within the nucleolus may prevent its proper recognition by specific antibodies , European Journal of Histochemistry: Vol. 49 No. 2 (2005)
- A Spano, L Sciola, G Monaco, S Barni, Relationship between actin microfilaments and plasma membrane changes during apoptosis of neoplastic cell lines in different culture conditions , European Journal of Histochemistry: Vol. 44 No. 3 (2000)
- E Farina Lipari, D Lipari, A Gerbino, D Di Liberto, M Bellafiore, M Catalano, B Valentino, The hypothalamic magnocellular neurosecretory system in developing rats , European Journal of Histochemistry: Vol. 45 No. 2 (2001)
<< < 69 70 71 72 73 74 75 76 77 78 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejh.2021.3228
https://doi.org/10.4081/ejh.2021.3228