Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Comparison of CGRP distributions in the maxillary sinus and trigeminal ganglion between elderly dentulous and edentulous humans
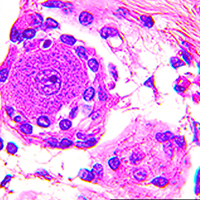
Thickening of the Schneiderian membrane (SM, mucosa of the maxillary sinus) appears in the paranasal sinus. Information on SM thickening is available for patients receiving sinus lift treatments, which is a risk factor for SM excretory dysfunction. However, more information is needed on the structure of the SM and the relationship between the maxilla sinus and palatine with the alveolar bone and the SM for dental implant treatment in the human maxilla. One hundred twenty-six sides of the maxilla from 71 cadavers were subjected to cone-beam CT (CBCT) analysis and macroscopic and immunohistochemical observations in this study. A thickened SM was mainly observed in the middle region of the basal layer of the maxillary sinus (MS). Strong calcitonin gene-related peptide (CGRP)-positive reactions were observed in the alveolar bone, oral mucosa, mucosa of the maxillary sinus, and trigeminal ganglion (TG) cells in dentulous samples compared with edentulous samples. TG cells play important roles in delivering CGRP through axons to the mucosal gland and in regulating the maxilla-related thickening of the SM. These data could help determine CGRP functions in the mucosal gland and bone formation between dentulous and edentulous samples and indicate that CGRP may pass from the TG to the maxillary sinus glands.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.