Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Immunohistochemistry as a paramount tool in research of normal urothelium, bladder cancer and bladder pain syndrome
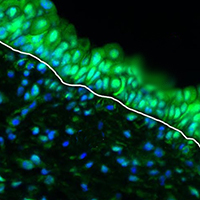
The urothelium, an epithelium of the urinary bladder, primarily functions as blood-urine permeability barrier. The urothelium has a very slow turn-over under normal conditions but is capable of extremely fast response to injury. During regeneration urothelium either restores normal function or undergoes altered differentiation pathways, the latter being the cause of several bladder diseases. In this review, we describe the structure of the apical plasma membrane that enables barrier function, the role of urothelium specific proteins uroplakins and the machinery for polarized membrane transports in terminally differentiated superficial umbrella cells. We address key markers, such as keratins, cancer stem cell markers, retinoic acid signalling pathway proteins and transient receptor potential channels and purinergic receptors that drive normal and altered differentiation in bladder cancer and bladder pain syndrome. Finally, we discuss uncertainties regarding research, diagnosis and treatment of bladder pain syndrome. Throughout the review, we emphasise the contribution of immunohistochemistry in advancing our understanding of processes in normal and diseased bladder as well as the most promising possibilities for improved bladder cancer and bladder pain syndrome management.
Supporting Agencies
Slovenian Research Agency ARRSHow to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.