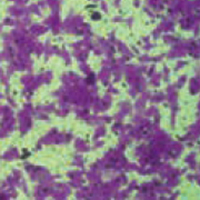
NOP14 regulates the growth, migration, and invasion of colorectal cancer cells by modulating the NRIP1/GSK-3β/β-catenin signaling pathway
Submitted: 15 March 2021
Accepted: 25 May 2021
Published: 2 July 2021
Accepted: 25 May 2021
Abstract Views: 1808
PDF: 549
HTML: 26
HTML: 26
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- G. Orsini, A. Majorana, A. Mazzoni, A. Putignano, M. Falconi, A. Polimeni, L. Breschi, Immunocytochemical detection of dentin matrix proteins in primary teeth from patients with dentinogenesis imperfecta associated with osteogenesis imperfecta , European Journal of Histochemistry: Vol. 58 No. 4 (2014)
- Zhongli Shi, Wayne K. Greene, Philip K. Nicholls, Dailun Hu, Janina E.E. Tirnitz-Parker, Qionglan Yuan, Changfu Yin, Bin Ma, Immunofluorescent characterization of non-myelinating Schwann cells and their interactions with immune cells in mouse mesenteric lymph node , European Journal of Histochemistry: Vol. 61 No. 3 (2017)
- K. Okamoto, N. Kiga, Y. Shinohara, I. Tojyo, S. Fujita, Effect of interleukin-1beta and dehydroepiandrosterone on the expression of lumican and fibromodulin in fibroblast-like synovial cells of the human temporomandibular joint , European Journal of Histochemistry: Vol. 59 No. 1 (2015)
- S. Nemolato, J. Ekstrom, T. Cabras, C. Gerosa, D. Fanni, E. Di Felice, A. Locci, I. Messana, M. Castagnola, G. Faa, Immunoreactivity for thymosin beta 4 and thymosin beta 10 in the adult rat oro-gastro-intestinal tract , European Journal of Histochemistry: Vol. 57 No. 2 (2013)
- M. Di Rosa, M.A. Szychlinska, D. Tibullo, L. Malaguarnera, G. Musumeci, Expression of CHI3L1 and CHIT1 in osteoarthritic rat cartilage model. A morphological study , European Journal of Histochemistry: Vol. 58 No. 3 (2014)
- F.S. De Ponte, G. Cutroneo, R. Falzea, G. Rizzo, L. Catalfamo, A. Favaloro, G. Vermiglio, M. Runci, A. Centofanti, G. Anastasi, Histochemical and morphological aspects of fresh frozen bone: a preliminary study , European Journal of Histochemistry: Vol. 60 No. 4 (2016)
- Andrea Conz, Clara Alice Musi, Luca Russo, Tiziana Borsello, Luca Colnaghi, Super-resolution study of PIAS SUMO E3-ligases in hippocampal and cortical neurons , European Journal of Histochemistry: Vol. 65 No. s1 (2021): Special Collection on Advances in Neuromorphology in Health and Disease
- C. Fede, G. Albertin, L. Petrelli, M.M. Sfriso, C. Biz, R. De Caro, C. Stecco, Expression of the endocannabinoid receptors in human fascial tissue , European Journal of Histochemistry: Vol. 60 No. 2 (2016)
- T. Karaca, Y. Hulya Uz, R. Karabacak, I. Karaboga, S. Demirtas, A. Cagatay Cicek, Effects of hyperthyroidism on expression of vascular endothelial growth factor (VEGF) and apoptosis in fetal adrenal glands , European Journal of Histochemistry: Vol. 59 No. 4 (2015)
- M. Aita, F. Benedetti, E. Carafelli, E. Caccia, N. Romano, Effects of hypophyseal or thymic allograft on thymus development in partially decerebrate chicken embryos: expression of PCNA and CD3 markers , European Journal of Histochemistry: Vol. 54 No. 3 (2010)
<< < 23 24 25 26 27 28 29 30 31 32 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejh.2021.3246
https://doi.org/10.4081/ejh.2021.3246











