Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Postsynaptic cleft density changes with combined exercise protocols in an experimental model of muscular hypertrophy
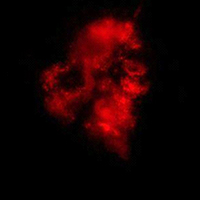
The vertical ladder-based protocols contribute to the NMJ junction's adaptations, and when combined with and without load, can be potentiated. The present study aimed to investigate postsynaptic regions of the biceps brachii muscle in adult male Wistar rats submitted to different vertical ladder-based protocols (Sedentary - S; Climbing - C; Climbing with Load - LC and Combined Climbing - CC). The protocols (C, LC, CC) were performed in 24 sessions, 3 x/week, for 8 weeks. The myofibrillar ATPase analysis showed an increase in cross-sectional area (CSA) of the muscle fibers Type I in all trained Groups; Type II in C and LC and reduction in CC; Type IIx higher in all trained Groups. In the postsynaptic cleft, the stained area presents smaller in Groups C, LC, and CC; the total area showed smaller than LC and higher in C and CC. The stained and total perimeter, and dispersion showed a reduction in C, LC, and CC, higher maximum diameter in Groups C and CC, and decreased in LC. Regarding the postsynaptic cleft distribution, the stained area presented a decrease in all trained Groups. The integrated density presented higher principally in CC. The NMJ count showed an increase in all trained Groups. We concluded that the vertical ladder-based protocols combined contributed to the postsynaptic region adaptations.
Downloads
Publication Facts
Reviewer profiles N/A
Author statements
- Academic society
- N/A
- Publisher
- PAGEPress Publications, Pavia, Italy
Supporting Agencies
FAPESP, Grants #2017/12525-1, #2017/21977-3, São Paulo Research Foundation (FAPESP), PROPG edital 05/2021, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Code 001How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2021.3274
https://doi.org/10.4081/ejh.2021.3274