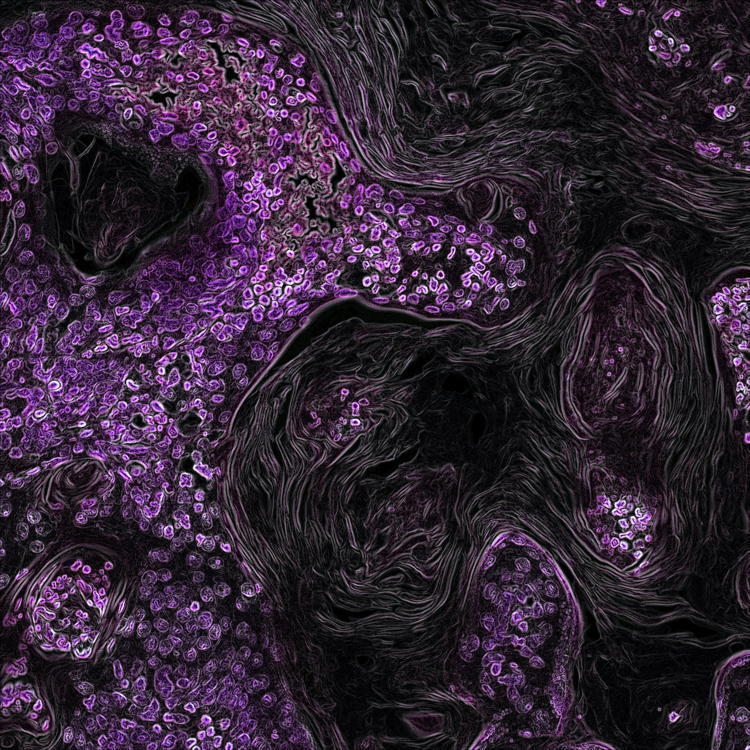
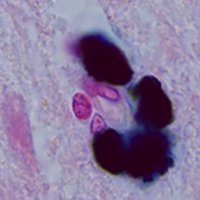
Changes in cytoplasmic and extracellular neuromelanin in human substantia nigra with normal aging
Submitted: 31 May 2021
Accepted: 22 July 2021
Published: 1 September 2021
Accepted: 22 July 2021
Abstract Views: 1042
PDF: 497
HTML: 12
HTML: 12
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- D. Curzi, S. Salucci, M. Marini, F. Esposito, L. Agnello, A. Veicsteinas, S. Burattini, E. Falcieri, How physical exercise changes rat myotendinous junctions: an ultrastructural study , European Journal of Histochemistry: Vol. 56 No. 2 (2012)
- W. Romero-Fernandez, D.O. Borroto-Escuela, V. Vargas-Barroso, M. Narváez, M. Di Palma, L.F. Agnati, J. Larriva Sahd, K. Fuxe, Dopamine D1 and D2 receptor immunoreactivities in the arcuate-median eminence complex and their link to the tubero-infundibular dopamine neurons , European Journal of Histochemistry: Vol. 58 No. 3 (2014)
- A Sun, S Noriki, Y Imamura, M Fukuda, Detection of cancer clones in human gastric adenoma by increased DNA-instability and other biomarkers , European Journal of Histochemistry: Vol. 47 No. 2 (2003)
- Editor in Chief, In memoriam of Prof. GianCarlo Panzica , European Journal of Histochemistry: Vol. 66 No. 3 (2022)
- Manuela Malatesta, Histological and Histochemical Methods - Theory and practice , European Journal of Histochemistry: Vol. 60 No. 1 (2016)
- V. Poletto, V. Galimberti, G. Guerra, V. Rosti, F. Moccia, M. Biggiogera, Fine structural detection of calcium ions by photoconversion , European Journal of Histochemistry: Vol. 60 No. 3 (2016)
- MG Rambotti, G Altissimi, A Spreca, Enzyme-ultracytochemical study of adenylate and guanylate cyclases in normal and pathologic human nasal mucosa , European Journal of Histochemistry: Vol. 48 No. 3 (2004)
- B Vitolo, MR Lidonnici, C Montecucco, A Montecucco, A new monoclonal antibody against DNA ligase I is a suitable marker of cell proliferation in cultured cell and tissue section samples , European Journal of Histochemistry: Vol. 49 No. 4 (2005)
- A Gigante, S Manzotti, C Bevilacqua, M Orciani, R Di Primio, M Mattioli-Belmonte, Adult mesenchymal stem cells for bone and cartilage engineering: effect of scaffold materials , European Journal of Histochemistry: Vol. 52 No. 3 (2008)
- D Marzioni, C Crescimanno, D Zaccheo, R Coppari, CB Underhill, M Castellucci, Hyaluronate and CD44 expression patterns in the human placenta throughout pregnancy , European Journal of Histochemistry: Vol. 45 No. 2 (2001)
<< < 49 50 51 52 53 54 55 56 57 58 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejh.2021.3283
https://doi.org/10.4081/ejh.2021.3283