Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Sporadic Creutzfeldt-Jakob disease: Real-Time Quaking Induced Conversion (RT-QuIC) assay represents a major diagnostic advance
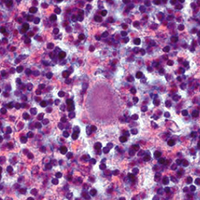
Sporadic Creutzfeldt-Jakob disease (sCJD) is a rare and fatal neurodegenerative disorder with an incidence of 1.5 to 2 cases per million population/year. The disease is caused by a proteinaceous infectious agent, named prion (or PrPSc), which arises from the conformational conversion of the cellular prion protein (PrPC). Once formed, PrPSc interacts with the normally folded PrPC coercing it to undergo similar structural rearrangement. The disease is highly heterogeneous from a clinical and neuropathological point of view. The origin of this variability lies in the aberrant structures acquired by PrPSc. At least six different sCJD phenotypes have been described and each of them is thought to be caused by a peculiar PrPSc strain. Definitive sCJD diagnosis requires brain analysis with the aim of identifying intracerebral accumulation of PrPSc which currently represents the only reliable biomarker of the disease. Clinical diagnosis of sCJD is very challenging and is based on the combination of several clinical, instrumental and laboratory tests representing surrogate disease biomarkers. Thanks to the advent of the ultrasensitive Real-Time Quaking-Induced Conversion (RT-QuIC) assay, PrPSc was found in several peripheral tissues of sCJD patients, sometimes even before the clinical onset of the disease. This discovery represents an important step forward for the clinical diagnosis of sCJD. In this manuscript, we present an overview of the current applications and future perspectives of RT-QuIC in the field of sCJD diagnosis.
Altmetrics
Downloads
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.