Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Immunoreactivity and a new staining method of monocarboxylate transporter 1 located in endothelial cells of cerebral vessels of human brain in distinguishing cerebral venules from arterioles
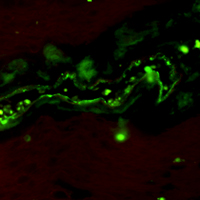
Distinguishing brain venules from arterioles with arteriolosclerosis is less reliable using traditional staining methods. We aimed to immunohistochemically assess the monocarboxylate transporter 1 (MCT1), a specific marker of venous endothelium found in rodent studies, in different caliber vessels in human brains. Both largeand small-caliber cerebral vessels were dissected from four autopsy donors. Immunoreactivity for MCT1 was examined in all autopsied human brain tissues, and then each vessel was identified by neuropathologists using hematoxylin and eosin stain, the Verhoeff’s Van Gieson stain, immunohistochemical stain with antibodies for α-smooth muscle actin and MCT1 in sequence. A total of 61 cerebral vessels, including 29 arteries and 32 veins were assessed. Immunoreactivity for MCT1 was observed in the endothelial cells of various caliber veins as well as the capillaries, whereas that was immunenegative in the endothelium of arteries. The different labeling patterns for MCT1 could aid in distinguishing various caliber veins from arteries, whereas assessment using the vessel shape, the internal elastic lamina, and the pattern of smooth muscle fibers failed to make the distinction between small-caliber veins and sclerotic arterioles. In conclusion, MCT1 immunohistochemical staining is a sensitive and reliable method to distinguish cerebral veins from arteries.
Downloads
Publication Facts
Reviewer profiles N/A
Author statements
- Academic society
- N/A
- Publisher
- PAGEPress Publications, Pavia, Italy
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2021.3306
https://doi.org/10.4081/ejh.2021.3306