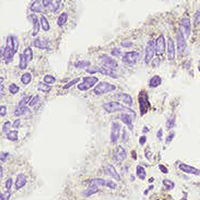
The lncRNA MEG3 promotes trophoblastic cell growth and invasiveness in preeclampsia by acting as a sponge for miR-21, which regulates BMPR2 levels
Submitted: 6 September 2021
Accepted: 19 October 2021
Published: 25 November 2021
Accepted: 19 October 2021
Abstract Views: 1016
PDF: 484
HTML: 22
HTML: 22
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- M Aita, E Carafelli, L Alfei, B Caronti, Thymic development in surgically bursectomized embryonic chicken: expression of PCNA, CD3, CD4 and CD8 markers , European Journal of Histochemistry: Vol. 51 No. 4 (2007)
- G Lingua, G D’Agostino, A Fusconi, G Berta, Nuclear changes in pathogen-infected tomato roots , European Journal of Histochemistry: Vol. 45 No. 1 (2001)
- L. Lanfranco, R. Balsamo, E. Martino, S. Perotto, P. Bonfante, Zinc ions alter morphology and chitin deposition in an ericoid fungus , European Journal of Histochemistry: Vol. 46 No. 4 (2002)
- D. Kluchova, A. Bolekova, C. Heichel, A. J. Bron, I. Kozak, NADPH-diaphorase expression in the Meibomian glands of rat palpebra in postnatal development , European Journal of Histochemistry: Vol. 54 No. 4 (2010)
- S Preziuso, E Sanna, MP Sanna, C Loddo, D Cerri, E Taccini, F Mariotti, G Braca, G Rossi, Association of Maedi Visna virus with Brucella ovis infection in rams , European Journal of Histochemistry: Vol. 47 No. 2 (2003)
- L Benkoël, P Biagini, F Dodero, X De Lamballerie, P De Micco, A Chamlian, D Lombardo, Immunohistochemical detection of C-100 hepatitis C virus antigen in formaldehyde-fixed paraffin-embedded liver tissue. Correlation with serum, tissue and in situ RT-PCR results , European Journal of Histochemistry: Vol. 48 No. 2 (2004)
- Monica Colitti, Federico Boschi, Tommaso Montanari, Dynamic of lipid droplets and gene expression in response to β-aminoisobutyric acid treatment on 3T3-L1 cells , European Journal of Histochemistry: Vol. 62 No. 4 (2018)
- D Tagu, R Marmeisse, Y Baillet, S Rivière, B Palin, F Bernardini, A Méreau, G Gay, R Balestrini, P Bonfante, F Martin, Hydrophobins in ectomycorrhizas: heterologous transcription of the Pisolithus HydPt-1 gene in yeast and Hebeloma cylindrosporum , European Journal of Histochemistry: Vol. 46 No. 1 (2002)
- CarloAlberto Redi, Calcium measurement methods , European Journal of Histochemistry: Vol. 54 No. 3 (2010)
- CarloAlberto Redi, Transcription factors - Methods and protocols , European Journal of Histochemistry: Vol. 55 No. 1 (2011)
<< < 75 76 77 78 79 80 81 82 83 84 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejh.2021.3323
https://doi.org/10.4081/ejh.2021.3323











