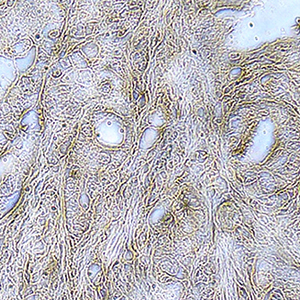
alpha2,3 sialic acid processing enzymes expression in gastric cancer tissues reveals that ST3Gal3 but not Neu3 are associated with Lauren's classification, angiolymphatic invasion and histological grade
Submitted: 16 September 2021
Accepted: 27 August 2022
Published: 29 September 2022
Accepted: 27 August 2022
Abstract Views: 822
PDF: 481
Supplementary: 76
HTML: 22
Supplementary: 76
HTML: 22
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- M. Malatesta, Skeletal muscle features in myotonic dystrophy and sarcopenia: do similar nuclear mechanisms lead to skeletal muscle wasting? , European Journal of Histochemistry: Vol. 56 No. 3 (2012)
- A. Arcucci, M.R. Ruocco, F. Albano, G. Granato, V. Romano, G. Corso, C. Bancone, E. De Vendittis, A. Della Corte, S. Montagnani, Analysis of extracellular superoxide dismutase and Akt in ascending aortic aneurysm with tricuspid or bicuspid aortic valve , European Journal of Histochemistry: Vol. 58 No. 3 (2014)
- Cecilia Dall'Aglio, Angela Polisca, Maria Grazia Cappai, Francesca Mercati, Alessandro Troisi, Carolina Pirino, Paola Scocco, Margherita Maranesi, Immunohistochemistry detected and localized cannabinoid receptor type 2 in bovine fetal pancreas at late gestation , European Journal of Histochemistry: Vol. 61 No. 1 (2017)
- A. Lee, A.R. Anderson, M. Stevens, S. Beasley, N.L. Barnett, D.V. Pow, Excitatory Amino Acid Transporter 5 is widely expressed in peripheral tissues , European Journal of Histochemistry: Vol. 57 No. 1 (2013)
- E Rossi, A Ubiali, P Balzarini, M Cadei, F Alpi, PG Grigolato, High-level detection of gene amplification and chromosome aneuploidy in extracted nuclei from paraffin-embedded tissue of human cancer using FISH: a new approach for retrospective studies , European Journal of Histochemistry: Vol. 49 No. 1 (2005)
- A. Di Giancamillo, M.E. Andreis, P. Taini, M.C. Veronesi, M. Di Giancamillo, S.C. Modina, Cartilage canals in newborn dogs: histochemical and immunohistochemical findings , European Journal of Histochemistry: Vol. 60 No. 3 (2016)
- Mohammed Akeel, Ahmed Elhafey , Atef Shehata , Erwa Elmakki , Thanaa Aboshouk, Hussein Ageely , Mohammed Salih Mahfouz , Efficacy of immunohistochemical staining in detecting Helicobacter pylori in Saudi patients with minimal and atypical infection , European Journal of Histochemistry: Vol. 65 No. 3 (2021)
- D. Ami, M. Di Segni, M. Forcella, V. Meraviglia, M. Baccarin, S.M. Doglia, G. Terzoli, Role of water in chromosome spreading and swelling induced by acetic acid treatment: a FTIR spectroscopy study , European Journal of Histochemistry: Vol. 58 No. 1 (2014)
- G. Tossetta, C. Avellini, C. Licini, S.R. Giannubilo, M. Castellucci, D. Marzioni, High temperature requirement A1 and fibronectin: two possible players in placental tissue remodelling , European Journal of Histochemistry: Vol. 60 No. 4 (2016)
- G Giuffrè, F Mormandi, V Barresi, C Bordi, G Tuccari, G Barresi, Quantity of AgNOR in gastric endocrine carcinoid tumours as a potential prognostic tool , European Journal of Histochemistry: Vol. 50 No. 1 (2006)
<< < 30 31 32 33 34 35 36 37 38 39 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejh.2022.3330
https://doi.org/10.4081/ejh.2022.3330











