Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
High expression of both desmoplastic stroma and epithelial to mesenchymal transition markers associate with shorter survival in pancreatic ductal adenocarcinoma
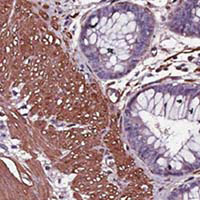
Desmoplastic stroma (DS) and the epithelial-to-mesenchymal transition (EMT) play a key role in pancreatic ductal adenocarcinoma (PDAC) progression. To date, however, the combined expression of DS and EMT markers, and their association with variations in survival within each clinical stage and degree of tumor differentiation is unknown. The purpose of this study was to investigate the association between expression of DS and EMT markers and survival variability in patients diagnosed with PDAC. We examined the expression levels of DS markers alpha smooth muscle actin (α-SMA), fibronectin, and vimentin, and the EMT markers epithelial cell adhesion molecule (EPCAM), pan-cytokeratin, and vimentin, by immunohistochemistry using a tissue microarray of a retrospective cohort of 25 patients with PDAC. The results were examined for association with survival by clinical stage and by degree of tumor differentiation. High DS markers expression -α-SMA, fibronectin, and vimentin- was associated with decreased survival at intermediate and advanced clinical stages (p=0.006-0.03), as well as with both poorly and moderately differentiated tumor grades (p=0.01-0.02). Interestingly, the same pattern was observed for EMT markers, i.e., EPCAM, pan-cytokeratin, and vimentin (p=0.00008-0.03). High expression of DS and EMT markers within each clinical stage and degree of tumor differentiation was associated with lower PDAC survival. Evaluation of these markers may have a prognostic impact on survival time variation in patients with PDAC.
Downloads
Publication Facts
Reviewer profiles N/A
Author statements
- Academic society
- N/A
- Publisher
- PAGEPress Publications, Pavia, Italy
Supporting Agencies
national science and technology council, coordination of health researchHow to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2022.3360
https://doi.org/10.4081/ejh.2022.3360