miR-19a targeting CLCA4 to regulate the proliferation, migration, and invasion of colorectal cancer cells
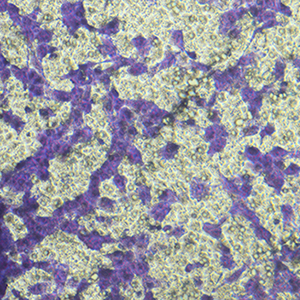
The role of miR-19a in colorectal cancer (CRC), a devastating disease with high mortality and morbidity, remains controversial. In the present study, we show that the level of miR-19a is significantly higher in clinical CRC tissue samples than in paracancerous tissue samples, and significantly higher in CRC cells lines HT29, SW480, and CaCO2 than in the normal human colon mucosal epithelial cell line NCM460. miR-19a mimics and inhibitors were synthesized and validated. Overexpression of miR-19a mimics significantly promoted, while miR-19a inhibitors inhibited, the proliferation, survival, migration, and invasion of SW480 and CaCO2 CRC cells. Furthermore, mRNA and protein levels of chloride channel accessory 4 (CLCA4) were lower in CRC cells and tissues. Bioinformatics and a luciferase reporter assay confirmed that CLCA4 was a miR-19a target. Further, miR-19a inhibition increased CLCA4 expression. The inhibitory effect of miR-19a on cell growth, survival, migration, and invasion was reversed by knockdown of CLCA4 expression. The data demonstrated that the miR-19a/CLCA4 axis modulates phospho-activation of the PI3K/AKT pathway in CRC cells. In conclusion, our results revealed that miR-19a overexpression decreases CLCA4 levels to promote CRC oncogenesis, suggesting that miR-19a inhibitors have potential applications for future therapeutic of CRC.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.