Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Ferroptosis resistance cooperates with cellular senescence in the overt stage of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis
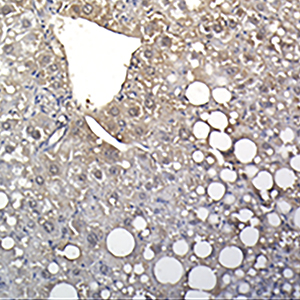
Cellular senescence and ferroptosis are the two main, fine-tuned processes in tissue damage restraint; however, they can be overactivated in pathologies such as nonalcoholic fatty liver disease/nonalcoholic steatohepatitis (NAFLD/NASH), becoming dangerous stimuli. Senescence is characterized by a decline in cell division and an abnormal release of reactive oxygen species (ROS), and ferroptosis is represented by iron deposition associated with an excessive accumulation of ROS. ROS and cellular stress pathways are also drivers of NAFLD/NASH development. The etiology of NAFLD/NASH lies in poor diets enriched in fat and sugar. This food regimen leads to liver steatosis, resulting in progressive degeneration of the organ, with a late onset of irreversible fibrosis and cirrhosis. Few studies have investigated the possible connection between senescence and ferroptosis in NAFLD/NASH progression, despite the two events sharing some molecular players. We hypothesized a possible link between senescence and ferroptosis in a NAFLD background. To thoroughly investigate this in the context of “Western-style” diet (WSD) abuse, we used an amylin-modified liver NASH mouse model. The main NASH hallmarks have been confirmed in this model, as well as an increase in apoptosis, and Ki67 and p53 expression in the liver. Senescent beta-galactosidase-positive cells were elevated, as well as the expression of the related secretory molecules Il-6 and MMP-1. Features of DNA damage and iron-overload were found in the livers of NASH mice. Gpx4 (glutathione peroxidase 4) expression, counteracting ferroptotic cell death, was increased. Notably, an increased number of senescent cells showing overexpression of gpx4 was also found. Our data seem to suggest that senescent cells acquire a gpx4-mediated mechanism of ferroptosis resistance and thus remain in the liver, fostering the deterioration of liver fitness.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.