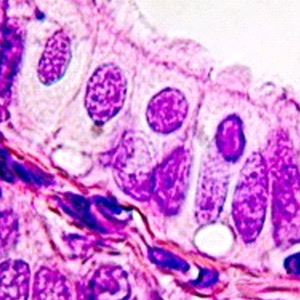
Molecules involved in the sperm interaction in the human uterine tube: a histochemical and immunohistochemical approach
Submitted: 16 October 2022
Accepted: 27 February 2023
Published: 13 April 2023
Accepted: 27 February 2023
Abstract Views: 715
PDF: 480
HTML: 35
HTML: 35
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Giulia Ronchi, Pierluigi Tos, Elia Angelino, Luisa Muratori, Simone Reano, Nicoletta Filigheddu, Andrea Graziani, Stefano Geuna, Stefania Raimondo, Effect of unacylated ghrelin on peripheral nerve regeneration , European Journal of Histochemistry: Vol. 65 No. s1 (2021): Special Collection on Advances in Neuromorphology in Health and Disease
- L Postiglione, G Di Domenico, G Giordano-Lanza, P Ladogana, M Turano, C Castaldo, Effect of human granulocyte macrophage-colony stimulating factor on differentiation and apoptosis of the human osteosarcoma cell line SaOS-2 , European Journal of Histochemistry: Vol. 47 No. 4 (2003)
- G Mazzini, C Ferrari, E Erba, Dual excitation multi-fluorescence flow cytometry for detailed analyses of viability and apoptotic cell transition , European Journal of Histochemistry: Vol. 47 No. 4 (2003)
- H. Zhang, P. Yu, S. Zhong, T. Ge, S. Peng, Z. Zhou, X. Guo, Gliocyte and synapse analyses in cerebral ganglia of the Chinese mitten crab, Eriocheir sinensis: ultrastructural study , European Journal of Histochemistry: Vol. 60 No. 3 (2016)
- Hitoshi Fujita, Kosuke Imura, Masahito Takiguchi, Kengo Funakoshi, Postnatal development of thalamic reticular nucleus projections to the anterior thalamic nuclei in rats , European Journal of Histochemistry: Vol. 66 No. 2 (2022)
- A. Sbarbati, D. Accorsi, D. Benati, L. Marchetti, G. Orsini, G. Rigotti, P. Panettiere, Subcutaneous adipose tissue classification , European Journal of Histochemistry: Vol. 54 No. 4 (2010)
- M. Malatesta, Skeletal muscle features in myotonic dystrophy and sarcopenia: do similar nuclear mechanisms lead to skeletal muscle wasting? , European Journal of Histochemistry: Vol. 56 No. 3 (2012)
- M.A. Khalili, M. Maione, M.G. Palmerini, S. Bianchi, G. Macchiarelli, S.A. Nottola, Ultrastructure of human mature oocytes after vitrification , European Journal of Histochemistry: Vol. 56 No. 3 (2012)
- Chaoyong Tian, Yang Yang, Yao Li, Fei Sun, Juan Qu, Dingjun Zha, Expression and localization of α2A-adrenergic receptor in the rat post-natal developing cochlea , European Journal of Histochemistry: Vol. 67 No. 3 (2023)
- B. Emde, A. Heinen, A. Gödecke, K. Bottermann, Wheat germ agglutinin staining as a suitable method for detection and quantification of fibrosis in cardiac tissue after myocardial infarction , European Journal of Histochemistry: Vol. 58 No. 4 (2014)
<< < 44 45 46 47 48 49 50 51 52 53 > >>
You may also start an advanced similarity search for this article.
Publication Facts
Metric
This article
Other articles
Peer reviewers
2
2.4
Reviewer profiles N/A
Author statements
Author statements
This article
Other articles
Data availability
N/A
16%
External funding
N/A
32%
Competing interests
N/A
11%
Metric
This journal
Other journals
Articles accepted
57%
33%
Days to publication
178
145
- Academic society
- N/A
- Publisher
- PAGEPress Publications, Pavia, Italy

 https://doi.org/10.4081/ejh.2023.3513
https://doi.org/10.4081/ejh.2023.3513












