Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
The Qi-Bang-Yi-Shen formula ameliorates renal dysfunction and fibrosis in rats with diabetic kidney disease via regulating PI3K/AKT, ERK and PPARγ signaling pathways
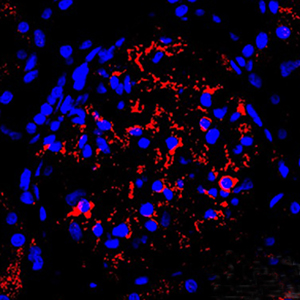
Diabetic kidney disease (DKD) is the leading cause of chronic kidney disease (CKD) and a growing public health problem worldwide. Losartan potassium (Los), an angiotensin II receptor blocker, has been used to treat DKD clinically. Recently, multi-herbal formula has been shown to exhibit therapeutic activities in DKD in China. Thus, we aimed to explore the protective effects of combination of Los and Qi-Bang-Yi-Shen formula (QBF) on DKD rats. Streptozotocin (STZ) injection was used to establish a rat model of DKD. Next, the bloodurea nitrogen (BUN), creatinine (CRE) and uric acid (UA) levels were detected in serum samples from DKD rats. Hematoxylin and eosin (H&E), periodic Acid Schiff (PAS) and Masson staining were performed to observe glomerular injury and glomerular fibrosis in DKD rats. In this study, we found that QBF or Los treatment could decrease serum BUN, CRE, UA levels and reduce urine albumin-to-creatinine ratio (ACR) in DKD rats. Additionally, QBF or Los treatment obviously inhibited glomerular mesangial expansion and glomerular fibrosis, attenuated glomerular injury in kidney tissues of DKD rats. Moreover, QBF or Los treatment significantly reduced PI3K, AKT and ERK1/2 protein expressions, but increased PPARγ level in kidney tissues of DKD rats. As expected, combined treatment of QBF and Los could exert enhanced reno-protective effects compared with the single treatment. Collectively, combination of QBF and Los could ameliorate renal injury and fibrosis in DKD rats via regulating PI3K/AKT, ERK and PPARγ signaling pathways. These findings highlight the therapeutic potential of QBF to prevent DKD progression.
Downloads
Publication Facts
Reviewer profiles N/A
Author statements
- Academic society
- N/A
- Publisher
- PAGEPress Publications, Pavia, Italy
Citations
10.3389/fphar.2025.1566723
10.3390/molecules28248030
10.1111/nep.14404
10.1155/2024/8772009
10.6039/j.issn.1001-0408.2024.14.22
10.56434/j.arch.esp.urol.20247702.24
Ethics Approval
This study was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital and conducted according to the international rules and guidelines.How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2023.3648
https://doi.org/10.4081/ejh.2023.3648