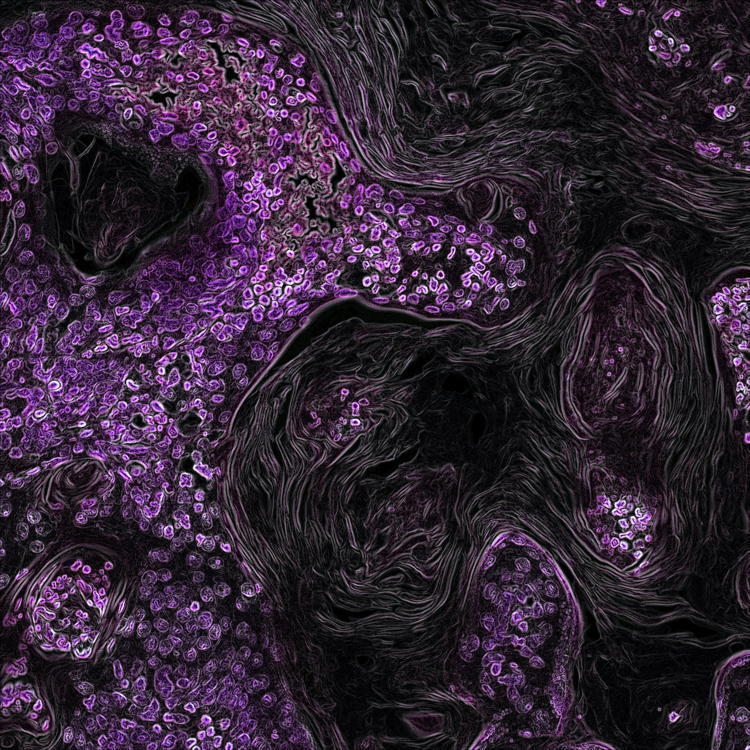
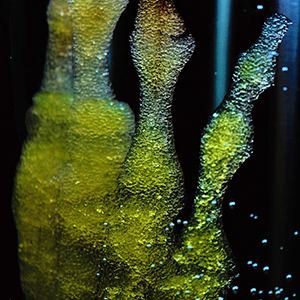
The contribution of immunohistochemistry to the development of hydrogels for skin repair and regeneration
Submitted: 9 February 2023
Accepted: 17 February 2023
Published: 23 February 2023
Accepted: 17 February 2023
Abstract Views: 916
PDF: 545
HTML: 22
HTML: 22
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Qichao Yin, Hua Xiong, Chemotherapy-induced nephrotoxicity was improved by crocin in mouse model , European Journal of Histochemistry: Vol. 66 No. 4 (2022)
- Daša Zupančič, Rok Romih, Immunohistochemistry as a paramount tool in research of normal urothelium, bladder cancer and bladder pain syndrome , European Journal of Histochemistry: Vol. 65 No. 2 (2021)
- Wenjing Liu, Shanshan Ming, Xiaobing Zhao, Xin Zhu, Yuxiang Gong, Developmental expression of high-mobility group box 1 (HMGB1) in the mouse cochlea , European Journal of Histochemistry: Vol. 67 No. 3 (2023)
- C. Dall'Oca, T. Maluta, F. Cavani, G.P. Morbioli, P. Bernardi, A. Sbarbati, D. Degl'Innocenti, B. Magnan, The biocompatibility of porous vs non-porous bone cements: a new methodological approach , European Journal of Histochemistry: Vol. 58 No. 2 (2014)
- Y. Liu, J. Weng, S. Huang, Y. Shen, X. Sheng, Y. Han, M. Xu, Q. Weng, Immunoreactivities of PPARγ2, leptin and leptin receptor in oviduct of Chinese brown frog during breeding period and pre-hibernation , European Journal of Histochemistry: Vol. 58 No. 3 (2014)
- Wanchun Wang, Jun Yi, Degang Dong, Wenli Mao, Xuanyu Wang, Zhangren Yan, miRNA-877-5p inhibits malignant progression of prostate cancer by directly targeting SSFA2 , European Journal of Histochemistry: Vol. 65 No. 3 (2021)
- S. He, J. Yang, Maturation of neurotransmission in the developing rat cochlea: immunohistochemical evidence from differential expression of synaptophysin and synaptobrevin 2 , European Journal of Histochemistry: Vol. 55 No. 1 (2011)
- A. Arcucci, M.R. Ruocco, F. Albano, G. Granato, V. Romano, G. Corso, C. Bancone, E. De Vendittis, A. Della Corte, S. Montagnani, Analysis of extracellular superoxide dismutase and Akt in ascending aortic aneurysm with tricuspid or bicuspid aortic valve , European Journal of Histochemistry: Vol. 58 No. 3 (2014)
- C.A. May, I. Osterland, Merkel cell distribution in the human eyelid , European Journal of Histochemistry: Vol. 57 No. 4 (2013)
- Matias Garrido, Camila Escobar, Constanza Zamora, Carolina Rejas, Juan Varas, Mario Párraga, Sebastián San Martin, Sandra Montedonico, Bile duct ligature in young rats: A revisited animal model for biliary atresia , European Journal of Histochemistry: Vol. 61 No. 3 (2017)
<< < 30 31 32 33 34 35 36 37 38 39 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejh.2023.3679
https://doi.org/10.4081/ejh.2023.3679