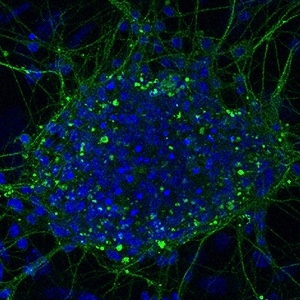
High glucose inhibits neural differentiation by excessive autophagy via peroxisome proliferator-activated receptor gamma
Submitted: 22 February 2023
Accepted: 24 April 2023
Published: 11 May 2023
Accepted: 24 April 2023
Abstract Views: 693
PDF: 568
HTML: 14
HTML: 14
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- V. Di Felice, G. Zummo, Stem cell populations in the heart and the role of Isl1 positive cells , European Journal of Histochemistry: Vol. 57 No. 2 (2013)
- Fenqiang Qi, Yuxin Deng, Wei Huang, Yanli Cai, Kelin Hong, Shui Xiang, Irisin suppresses PDGF-BB-induced proliferation of vascular smooth muscle cells in vitro by activating AMPK/mTOR-mediated autophagy , European Journal of Histochemistry: Vol. 68 No. 4 (2024)
- Gianluca Accogli, Giovanni Scillitani, Donatella Mentino, Salvatore Desantis, Characterization of the skin mucus in the common octopus Octopus vulgaris (Cuvier) reared paralarvae , European Journal of Histochemistry: Vol. 61 No. 3 (2017)
- Menghui Chen, Su Liu, Atorvastatin reduces calcification in valve interstitial cells via the NF-κB signalling pathway by promoting Atg5-mediated autophagy , European Journal of Histochemistry: Vol. 68 No. 2 (2024)
- Arianna Casini, Romina Mancinelli, Caterina Loredana Mammola, Luigi Pannarale, Piero Chirletti, Paolo Onori, Rosa Vaccaro, Distribution of alpha-synuclein in normal human jejunum and its relations with the chemosensory and neuroendocrine system , European Journal of Histochemistry: Vol. 65 No. 4 (2021)
- S. Strobel, J.A. Encarnação, N.I. Becker, T.E. Trenczek, Histological and histochemical analysis of the gastrointestinal tract of the common pipistrelle bat (Pipistrellus pipistrellus) , European Journal of Histochemistry: Vol. 59 No. 2 (2015)
- W.J. Liu, J. Yang, Developmental expression of inositol 1, 4, 5-trisphosphate receptor in the post-natal rat cochlea , European Journal of Histochemistry: Vol. 59 No. 2 (2015)
- H. Zhang, X. Guo, S. Zhong, T. Ge, S. Peng, P. Yu, Z. Zhou, Heterogeneous vesicles in mucous epithelial cells of posterior esophagus of Chinese giant salamander (Andrias davidianus) , European Journal of Histochemistry: Vol. 59 No. 3 (2015)
- Jindong Li, Jie Kang, Weiyan Liu, Jiazhe Liu, Gaofeng Pan, Anwei Mao, Qing Zhang, Jingfeng Lu, Junbin Ding, Hongchang Li, Docetaxel-resistant triple-negative breast cancer cell-derived exosomal lncRNA LINC00667 reduces the chemosensitivity of breast cancer cells to docetaxel via targeting miR-200b-3p/Bcl-2 axis , European Journal of Histochemistry: Vol. 66 No. 4 (2022)
- Xiangjun Lu, Jian Shen, Siyuan Huang, Dongdong Liu, Haitao Wang, Tumor cells-derived exosomal PD-L1 promotes the growth and invasion of lung cancer cells in vitro via mediating macrophages M2 polarization , European Journal of Histochemistry: Vol. 67 No. 3 (2023)
<< < 1 2 3 4 5 6 7 8 9 10 > >>
You may also start an advanced similarity search for this article.
Publication Facts
Metric
This article
Other articles
Peer reviewers
3
2.4
Reviewer profiles N/A
Author statements
Author statements
This article
Other articles
Data availability
N/A
16%
External funding
N/A
32%
Competing interests
N/A
11%
Metric
This journal
Other journals
Articles accepted
57%
33%
Days to publication
77
145
- Academic society
- N/A
- Publisher
- PAGEPress Publications, Pavia, Italy

 https://doi.org/10.4081/ejh.2023.3691
https://doi.org/10.4081/ejh.2023.3691












