Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
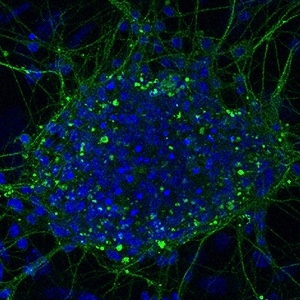
High glucose inhibits neural differentiation by excessive autophagy via peroxisome proliferator-activated receptor gamma
The high prevalence of prediabetes and diabetes globally has led to the widespread occurrence of severe complications, such as diabetic neuropathy, which is a result of chronic hyperglycemia. Studies have demonstrated that maternal diabetes can lead to neural tube defects by suppressing neurogenesis during neuroepithelium development. While aberrant autophagy has been associated with abnormal neuronal differentiation, the mechanism by which high glucose suppresses neural differentiation in stem cells remains unclear. Therefore, we developed a neuronal cell differentiation model of retinoic acid induced P19 cells to investigate the impact of high glucose on neuronal differentiation in vitro. Our findings indicate that high glucose (HG) hinders neuronal differentiation and triggers excessive. Furthermore, HG treatment significantly reduces the expression of markers for neurons (Tuj1) and glia (GFAP), while enhancing autophagic activity mediated by peroxisome proliferator-activated receptor gamma (PPARγ). By manipulating PPARγ activity through pharmacological approaches and genetically knocking it down using shRNA, we discovered that altering PPARγ activity affects the differentiation of neural stem cells exposed to HG. Our study reveals that PPARγ acts as a downstream mediator in high glucose-suppressed neural stem cell differentiation and that refining autophagic activity via PPARγ at an appropriate level could improve neuronal differentiation efficiency. Our data provide novel insights and potential therapeutic targets for the clinical management of gestational diabetes mellitus.
Ethics Approval
This study received approval from the Ethics Committee of Jinan University (approval no. 20210826-25; Guangzhou, China)How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.