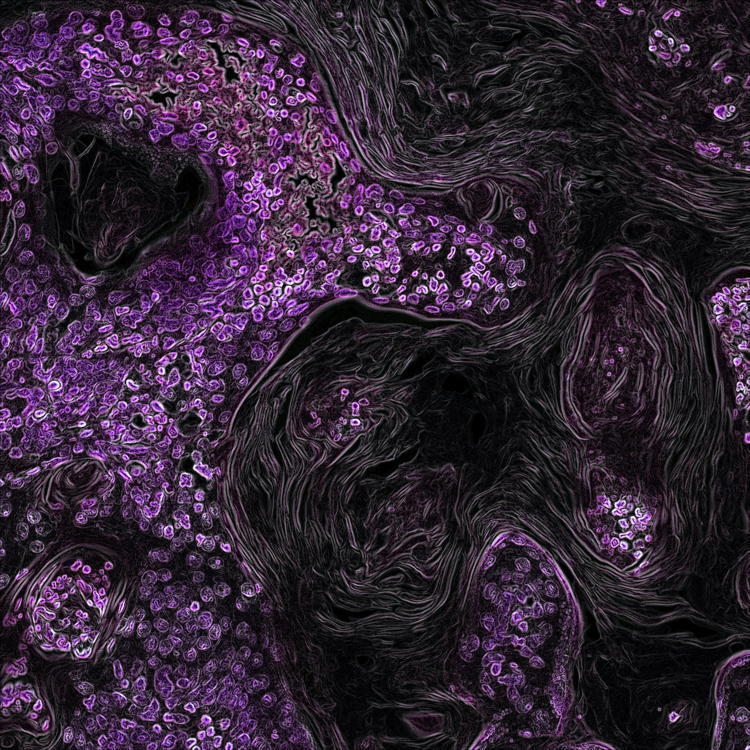
Astragaloside IV augments anti-PD-1 therapy to suppress tumor growth in lung cancer by remodeling the tumor microenvironment
Submitted: 30 June 2024
Accepted: 22 August 2024
Published: 23 October 2024
Accepted: 22 August 2024
Abstract Views: 426
PDF: 85
HTML: 0
HTML: 0
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Carlo Alberto Redi, Regenerating the heart - Stem cells and the cardiovascular system , European Journal of Histochemistry: Vol. 56 No. 2 (2012)
- RG Steinbeck, Dysplasia in view of the cell cycle , European Journal of Histochemistry: Vol. 48 No. 3 (2004)
- G Tuccari, G Giuffrè, R Scarfì, A Simone, P Todaro, G Barresi, Immunolocalization of lactoferrin in surgically resected pigmented skin lesions , European Journal of Histochemistry: Vol. 49 No. 1 (2005)
- A Zulli, LM Burrell, BF Buxton, DL Hare, ACE2 and AT4R are present in diseased human blood vessels , European Journal of Histochemistry: Vol. 52 No. 1 (2008)
- K Tatsuyama, Y Maezawa, H Baba, Y Imamura, M Fukuda, Expression of various growth factors for cell proliferation and cytodifferentiation during fracture repair of bone , European Journal of Histochemistry: Vol. 44 No. 3 (2000)
- Carlo Alberto Redi, Stem cells and aging - methods and protocols , European Journal of Histochemistry: Vol. 57 No. 3 (2013)
- Tingting Ge, Yaqiong Ye, Hui Zhang, Ultrastructure of telocytes, a new type of interstitial cells in the myocardium of the Chinese giant salamander (Andrias davidianus) , European Journal of Histochemistry: Vol. 63 No. 2 (2019)
- S Modina, M Beretta, V Lodde, A Lauria, AM Luciano, Cytoplasmic changes and developmental competence of bovine oocytes cryopreserved without cumulus cells , European Journal of Histochemistry: Vol. 48 No. 4 (2004)
- K Smetana, M Zápotocky´, J Starková, J Trka, To the nucleolar density and size in apoptotic human leukemic myeloblasts produced in vitro by Trichostatin A , European Journal of Histochemistry: Vol. 52 No. 3 (2008)
- Hitoshi Fujita, Kosuke Imura, Masahito Takiguchi, Kengo Funakoshi, Postnatal development of thalamic reticular nucleus projections to the anterior thalamic nuclei in rats , European Journal of Histochemistry: Vol. 66 No. 2 (2022)
<< < 64 65 66 67 68 69 70 71 72 73 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/ejh.2024.4098
https://doi.org/10.4081/ejh.2024.4098










